Case A
This case study follows a female patient in her sixties who visited our office approximately three years ago due to a fractured tooth (number eight) near the gum line. Initially advised for an implant, she opted to repeatedly re-cement the tooth every six months. However, after experiencing increasing pain and discovering a root crack, she decided to proceed with an implant and partial extraction therapy to address gingival height and bone loss concerns. Additionally, she chose to undergo four anterior veneers for aesthetic enhancement.
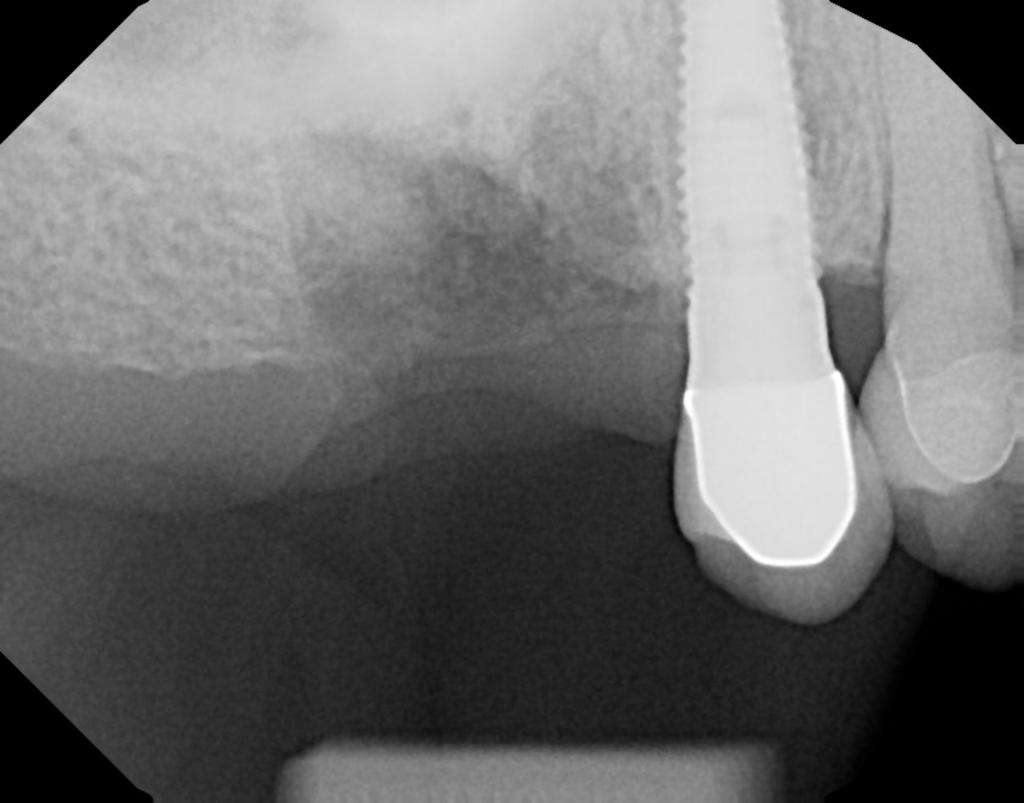
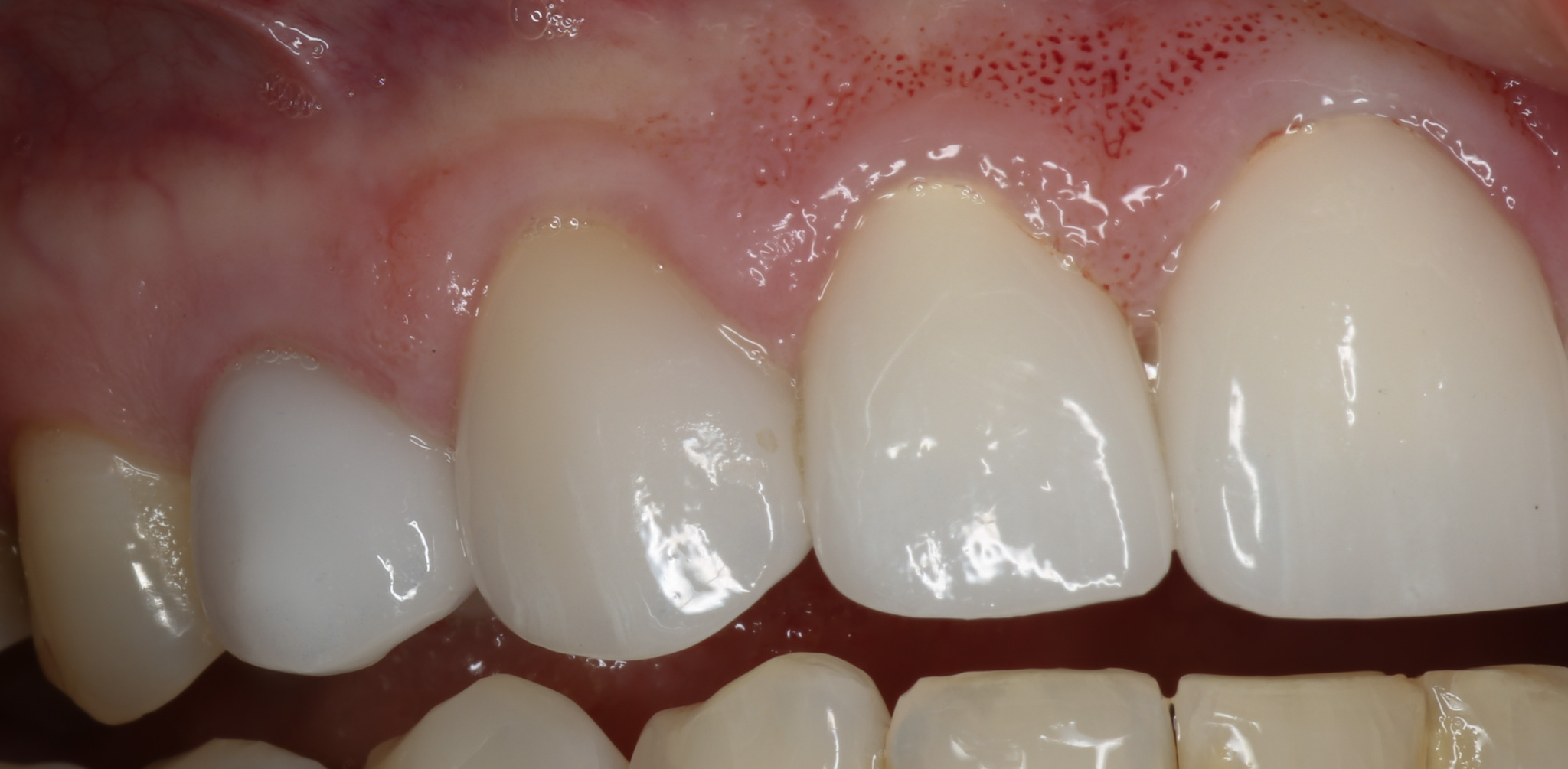
In the initial photo, tooth number eight is visibly broken at the gum line, with insufficient structure for retention. We opted to preserve the existing root structure due to its favorable height. Following implant placement and partial extraction therapy, subsequent images illustrate successful integration with surrounding teeth. Five months post-procedure, the final result exhibits seamless blending with natural teeth, with the zirconium abutment mimicking a natural root structure.




Case B
This patient presented with a draining fistula due to a blown-out root canal, necessitating tooth extraction. Opting for an “All-In-Implant™” approach, the procedure was meticulously planned in NemoScan software.
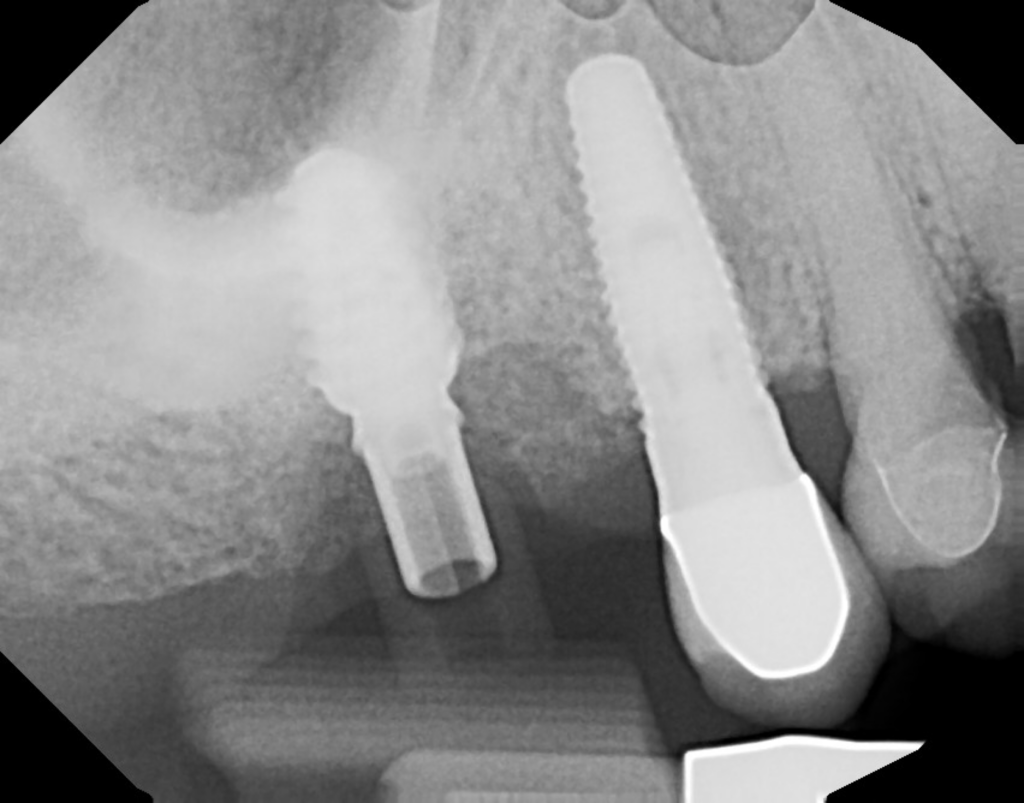
Image 26 captures the day of surgery with the abutment in place, showing initial healing with some erythema around the site. Despite anticipated gum recession, the abutment fit precisely within the socket dimensions, promoting optimal healing.
Three to four months post-surgery (image 24), significant bone growth was observed around the implant, indicating successful integration. The final crown (image 25), placed after one year of service, demonstrated preserved buccal bone and papilla, maintaining the natural emergence profile.
This case exemplifies the efficacy of comprehensive treatment planning and precise execution in achieving long-term dental health and aesthetics for patients with challenging conditions.




Case C
A 90-year-old patient presented with severe tooth decay resulting in loss of tooth structure and compromised bone density. Given his age and the importance of maintaining oral function for quality of life, we opted for a conservative approach. After careful evaluation, we performed a sinus lift and placed a custom healing abutment to support the implant.
One week post-procedure, slight gum recession was observed, but subsequent healing was favorable. The final crown restoration effectively restored Mr. McRae’s ability to eat comfortably, enhancing his enjoyment of life in his later years. Despite initial doubts about the procedure’s suitability for his age, the successful outcome demonstrates the importance of tailored treatment plans based on individual patient needs and desires.



Case D
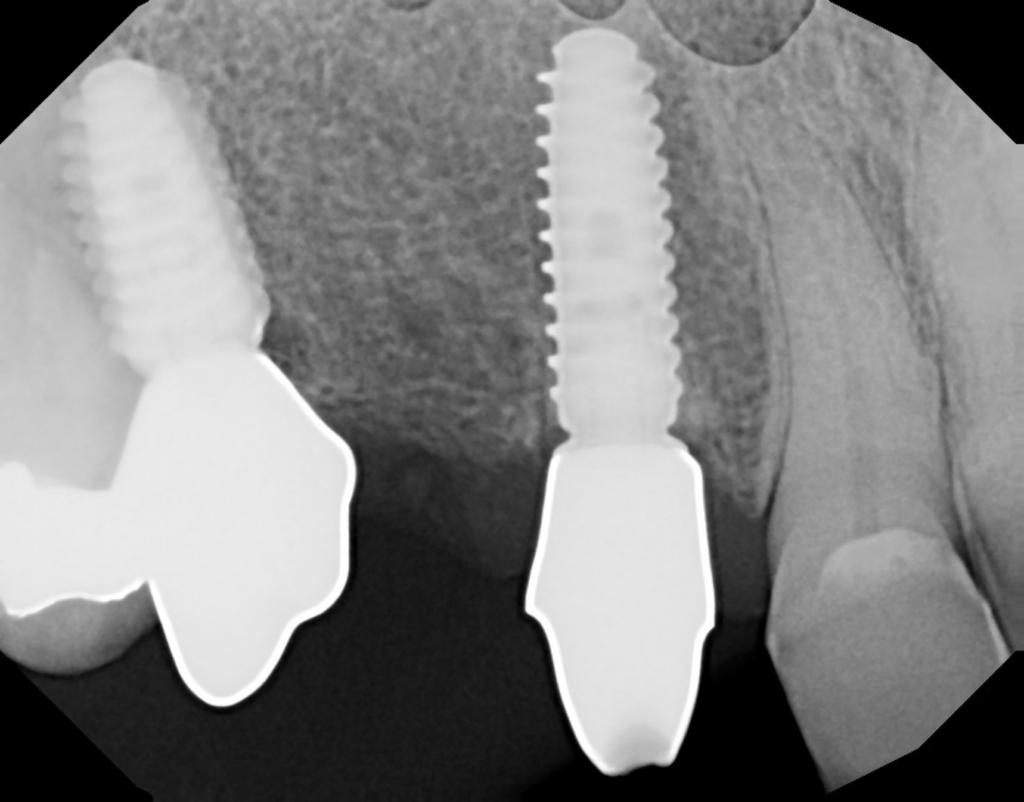
This patient sought treatment for decay beneath the gum line, opting for extraction and immediate implant placement over root canal therapy. The procedure included socket sealing with an abutment on the day of surgery, with minor mesial opening noted. She wore a temporary crown for four months post-surgery.
Remarkably, she experienced zero pain throughout the procedure and recovery period. The socket sealing technique contributed to reduced discomfort and facilitated bone healing. At the three-month mark, platform switching enhanced bone sealing around the implant. The continuous presence of the abutment ensured improved sealing and patient comfort throughout the healing process.




Case E
Patient E, a dental assistant in her 40s, sought veneer replacement but was found to have an abscess in tooth number five upon diagnostic imaging. Given the extent of root involvement, partial extraction therapy (PET) was deemed necessary. This involved extraction of the majority of the root followed by implant placement and bone grafting.
The final abutment, although effectively sealing the socket, required minor gingival adjustment for optimal integration. Despite a color mismatch with existing teeth due to a lab error, the outcome six months post-surgery was both aesthetically pleasing and functionally sound.
Advanced planning software ensured precise implant placement, aligning with the intended occlusion and contact points. This meticulous approach contributed to the successful restoration and highlights the complexity and precision achievable in contemporary dental procedures.



Case F
Patient F presented with a fractured bridge and two remaining roots, seeking restoration options after visiting multiple providers over several years. A treatment plan involving two implants with partial extraction therapy (PET) was proposed and executed.
Utilizing comprehensive guides for tissue reduction, PET, and surgical implant placement, the procedure achieved successful abutment placement with implant stability exceeding minimum requirements. Post-surgery, excellent gingival height and aesthetics were achieved, resulting in high patient satisfaction.
Despite the bridge-like appearance due to connecting the implants, the outcome closely resembled natural dentition. This case underscores the effectiveness of guided implant procedures in restoring function and aesthetics for patients with complex dental needs.


Case G
In a complex Nobel Guide case, a patient insisted on veneers despite root resorption in teeth 9 and 10 due to previous orthodontic treatment. Tooth 10 was mobile and required extraction, while tooth 9 was retained with splinted veneers. A Nobel Active implant was placed for tooth 10, with the final abutment and gum lift for tooth 11 performed on the same day.
Image 25 depicts the successful finalization of tooth 10. While not an “All-In-Implant™” case, meticulous planning and execution were required, particularly in coordinating the timing of the abutment placement. Despite the challenges, the outcome demonstrated effective restoration in a demanding aesthetic case.


